Patient Resources
Your Shoulder
Arthroscopic Surgery
 In the past, treatment of orthopedic injuries involved extensive surgery,
including large incisions, a hospital stay and a prolonged recovery period.
But arthroscopy has revolutionized the treatment of joint injuries.
In the past, treatment of orthopedic injuries involved extensive surgery,
including large incisions, a hospital stay and a prolonged recovery period.
But arthroscopy has revolutionized the treatment of joint injuries.
With the help of an arthroscope, today's orthopedic surgeons can easily
examine, diagnose, and treat problems in the joint that previously may
have been difficult to identify.
The arthroscope is a small fiber-optic viewing instrument made up of a
tiny lens, light source and video camera.
 diameter), but appear much larger when viewed through an arthroscope. This is a probe
used for examination of internal structures.
diameter), but appear much larger when viewed through an arthroscope. This is a probe
used for examination of internal structures.
The surgeon inserts the arthroscope into the joint through a tiny incision (about 1/4 of an
inch) called a portal. Other portals are used for the insertion of surgical instruments.
Anatomy of the Shoulder
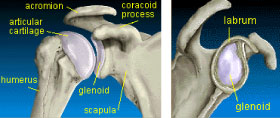 The two main bones of the shoulder are the humerus
and the scapula (shoulder blade). The end of the
scapula, called the glenoid, meets the head of the
humerus to form a glenohumeral cavity that acts as a
flexible ball-and-socket joint.
The two main bones of the shoulder are the humerus
and the scapula (shoulder blade). The end of the
scapula, called the glenoid, meets the head of the
humerus to form a glenohumeral cavity that acts as a
flexible ball-and-socket joint.
The joint cavity is cushioned by articular cartilage
covering the head of the humerus and face of the
glenoid. The scapula extends up and around the
shoulder joint at the rear to form a roof called the acromion, and around the shoulder joint at the front to form
the coracoid process.
 A ring of fibrous cartilage surrounds the glenoid and stabilizes
the joint. This is called the labrum.
A ring of fibrous cartilage surrounds the glenoid and stabilizes
the joint. This is called the labrum.
Ligaments connect the bones of the shoulder and tendons join
the bones to surrounding muscles.
The biceps tendon attaches the biceps muscle to the shoulder
and helps to stabilize the joint.
Four short muscles originate on the scapula and pass around the shoulder where their tendons fuse together
to form the rotator cuff.
All of these components of your shoulder, along with the muscles of your upper body, work together to
manage the stress your shoulder receives as you extend, flex, lift and throw.
Rotator Cuff Tears
1. What is the rotator cuff in the shoulder?
The rotator cuff is a group of flat tendons that fuse together and surround the front, back and top of the
shoulder joint like a cuff on a shirt sleeve. These tendons are connected individually to short - but very
important - muscles that originate from the scapula. When the muscles contract, they pull on the rotator cuff
tendon, causing the shoulder to rotate upward, inward or outward - hence the name "rotator cuff."
2. What is impingement syndrome?
The uppermost tendon of the rotator cuff (the supraspinatus tendon) passes beneath the bone on the top of
the shoulder, called the acromion. In some people, the space between the undersurface of the acromion and
the top of the humeral head is quite narrow. The rotator cuff tendon and the adherent bursa (or lubricating
tissue) can therefore be pinched when the arm is raised into a forward position. With repetitive impingement,
the tendons and bursa can become inflamed and swollen and cause the painful situation known as "chronic
impingement syndrome."
3. How does impingement syndrome relate to rotator cuff disease?
When the rotator cuff tendon and its overlying bursa become inflamed and swollen with impingement
syndrome, the tendon may begin to break down near its attachment on the humerus bone. With continued
impingement, the tendon is progressively damaged, and finally, may tear completely away from the bone.
4. Why do some people develop impingement and rotator cuff disease when others do not?
There are many factors that may predispose one person to impingement and rotator cuff problems. The
most common is the shape and thickness of the acromion (the bone forming the roof of the shoulder). If the
acromion has a bone spur on the front edge, it is more likely to impinge on the rotator cuff when the arm is
elevated forward. Activities that involve forward elevation of the arm may put an individual at higher risk for
rotator cuff injury. Sometimes the muscles of the shoulder may become imbalanced by injury or atrophy, and
imbalance can cause the shoulder to move forward with certain activities that again may cause impingement.
5. Other than impingement, what else can cause rotator cuff damage?
In young, athletic individuals, injury to the rotator cuff can occur with repetitive throwing, overhead racquet
sports or swimming. This type of injury results from repetitive stretching of the rotator cuff during the followthrough
phase of the activity. The tear that occurs is not caused by impingement, but more by a joint
imbalance. This may be associated with looseness in the front of the shoulder caused by a weakness in the
supporting ligaments.
6. What kind of symptoms does a patient have when the rotator cuff is injured?
The most common complaint is aching located in the top and front of the shoulder, or on the outer side of
the upper arm (deltoid area). The pain is usually increased when the arm is lifted to the overhead position.
Frequently, the pain seems to be worse at night and often interrupts sleep. Depending on the severity of the
injury, there may also be weakness in the arm and, with some complete rotator cuff tears, the arm cannot be
lifted in the forward or outward direction at all.
7. How is the diagnosis of rotator cuff disease proven?
The diagnosis of rotator cuff tendon disease includes a careful history taken and reviewed by the physician,
an x-ray to visualize the anatomy of the bones of the shoulder, specifically looking for acromial spur, and a
physical examination. Atrophy may be present, along with weakness, if the rotator cuff tendons are injured,
and special impingement tests can suggest that impingement syndrome is involved. An MRI (magnetic
resonance imaging) scan frequently gives the final proof of the status of the rotator cuff tendon. Although
none of these tests is guaranteed accurate, most rotator cuff injuries can be diagnosed using this combination
of exams.
8. What is the initial treatment for rotator cuff disease and impingement?
If minor impingement or rotator cuff tendinitis is diagnosed, a period of rest coupled with medicines and
physical therapy will frequently decrease the inflammation and restore the tone to the atrophied muscles.
Activities causing the pain should be slowly resumed only when the pain is gone. Sometimes a cortisone
injection into the bursal space above the rotator cuff tendon is helpful to relieve swelling and inflammation.
Application of ice to the tender area three or four times a day for 15 minutes is also helpful.
9. What is the second line of treatment if the rotator cuff pain and weakness persist?
If there is a thickened acromion or acromial bone spur causing impingement, it can be removed with a burr
using arthroscopic visualization. This procedure can often be performed on an outpatient basis, and at
the same time, any minor damage and fraying to the rotator cuff tendon and scarred bursal tissue can be
removed. Often this will completely cure the impingement and prevent progressive rotator cuff injury.
10. If the rotator cuff is already torn, what are the options?
When the tendon of the rotator cuff has a complete tear, the tendon often must be repaired using surgical
techniques. The choice of surgery depends on the severity of the symptoms, the health of the patient and
the functional requirements for that shoulder. In young working individuals, repair of the tendon is most often
suggested. In some older individuals who do not require significant overhead lifting ability, surgical repair may
not be as important. If chronic pain and disability are present at any age, consideration for repair of the rotator
cuff should be given.
11. What will happen if the rotator cuff is not repaired?
In some situations, the bursa overlying the rotator cuff may form a patch to close the defect in the tendon.
Although this is not true tendon healing, it may decrease the pain to an acceptable level. If the tendon edges
become fragmented and severely worn, and the muscle contracts and atrophies, repair at that point may
not be possible. Sometimes in this situation, the only beneficial surgical procedure would be an arthroscopic
operation to remove bone spurs and fragments of torn tissue that catch when the arm is rotated. This certainly
will not restore normal power or strength to the shoulder, but often will relieve pain.
12. How is a major injury to the rotator cuff tendon repaired surgically?
The arthroscope is extremely helpful when repairing rotator cuff tendons, but sometimes it is necessary to
add a "mini-open" procedure if the tendon is completely torn. Using the arthroscope at the beginning of the
case allows visualization of the interior of the joint to facilitate trimming and removal of fragments of torn cuff
tendon and biceps tendon. The next step utilizes the arthroscope to visualize the spur and thickened ligament
beneath the acromial bone, while they are removed with miniature cutting and grinding instruments. If it is
necessary to suture a rotator cuff tear that has pulled off the bone, a two-inch incision can be made directly
over the tear that has been visualized and localized using the arthroscope. The deltoid muscle fibers can be
spread apart so that strong stitches can attach the rotator cuff tendon back to the bone. If the tear is minimally
retracted, small suture screw anchors may be used arthroscopically or open.
13. How is my shoulder treated after surgery?
In a minor operation for impingement, the shoulder is placed in a simple sling. If a full thickness tear of
the rotator cuff was present and repaired, then an UltraSling or a SCOI postoperative brace supports the
shoulder. The brace is very helpful because it will allow exercise of the elbow, wrist, and hand at all times, and
places the arm in a position that promotes better blood circulation and relieves stress on the repaired rotator
cuff tissues. In addition, the shoulder can be exercised in the brace much easier than when it is at the side in
an immobilizer.
14. What is the rehabilitation program after rotator cuff surgery?
Depending on the type of surgery performed, the program will allow a period of time for healing of the soft
tissues followed by time to regain range of motion and then strengthen the shoulder muscles, but particularly
the rotator cuff. In minor tendinitis and impingement syndrome, the program takes approximately two to
three months. If the rotator cuff tendon has been completely torn, it may take six months or more before the
atrophied muscles can resume their function and the range of motion of the arm is restored. Frequently, pain
relief is much quicker and return to daily activities is often possible by two to three months.
15. How successful is rotator cuff surgery?
Again, every case is unique. In a young, healthy person with a minor rotator cuff impingement, surgery is
predictably successful. As the injury becomes more severe, such as with a large bone spur and fragmentation
of the tendon, a perfect result cannot be expected. Since it is necessary to trim back the unhealthy tendon
before reattaching it to the bone, a decreased range of motion of the shoulder will often result. Despite this,
pain relief and return of strength are usually well worth the minor decreased mobility. The final outcome often
depends on the willingness and ability of an individual patient to work on their postoperative physical therapy
program.
Shoulder Instability
Shoulder instability represents a spectrum of disorders, the successful management of which requires a
correct diagnosis and treatment. The boundaries of this spectrum are represented by a subluxation event (a
partial dislocation which spontaneously reduces), to a complete dislocation, which often requires anesthesia
to reduce the shoulder. The majority of instabilities are traumatic in nature and the ball of the shoulder is
unstable toward the front of the shoulder. It is this type of shoulder instability that we will concentrate on here.
In order for a shoulder to dislocate, the very important and delicate balance of soft tissues (ligaments, capsule
and tendons) around the shoulder become damaged. These damaged tissues often don't heal properly and
the shoulder can develop recurrent dislocations and/or pain with certain types of activities.
The older a patient is at the time of initial injury the lower the chances are for developing recurrent instability.
Patients under the age of 20 with traumatic dislocations have a substantially higher rate of recurrence (greater
than 90%). It is for this reason we have become more aggressive in recent years in recommending early
repair for this group of patients. We believe early repair reduces the likelihood of further injuring the shoulder
with additional episodes of dislocation.
The treatment for recurrent shoulder instability is usually surgical. This surgery is aimed at repairing the
damaged capsule and ligaments directly. This procedure can be done arthroscopically as an outpatient. The
surgery is performed with a miniature lighted telescope and small instruments introduced into the shoulder
joint through hollow cannulas. Advanced miniature anchors with suture attached are inserted precisely into
the socket of the shoulder, and the torn ligaments are reattached to the socket. Complete healing from this
procedure takes approximately 4-6 months.
Calcium deposits
Calcium deposits around the shoulder are a fairly common occurrence. Frequently they do not cause
problems, but if they increase in size or become inflamed, then very severe pain may result. This collection of
questions and answers is intended to explain this common shoulder problem and describe the methods we
recommend for treatment in different situations.
What is the cause of calcium deposits around the shoulder?
In most situations, there is no known cause for calcium deposits. Many people ask if their diet should
be changed to reduce calcium intake. This should never be used as a form of treatment, since a normal
balanced diet with a calcium supplement up to 1000mg a day is healthy in a normal patient, particularly senior
citizens and post-menopausal females.
Who most commonly gets calcium deposits?
Calcium deposits occur most frequently in females between 35 and 65 years of age, but may occur in males
as well.
Do all calcium deposits cause problems?
Many calcium deposits are present for years without causing any symptoms. Only when the deposit becomes
large enough to pinch between the bones when the shoulder is elevated, does it cause pain. Sometimes
smaller deposits cause pain if they become acutely inflamed, especially when the calcium salts leak from the
lesion into the sensitive bursal tissues.
Does a calcium deposit damage my shoulder?
Some calcium deposits can cause erosion with the destruction of a portion of the rotator cuff tendon. Most
calcium deposits remain on the outside of the rotator cuff tendon in the bursa and only cause problems
because of their pain and catching.
Is the calcium deposit hard like a rock?
Most early calcium deposits are very soft like toothpaste, but sometimes after being present for a long period
of time, they do dry up and become chalk-like, sometimes even turning to bone.
What is the best treatment for a calcium deposit?
When a calcium deposit becomes acutely inflamed, either because it ruptures and leaks calcium salts into
the bursa, or because it pinches the bursa or rotator cuff, the symptoms can be quite severe. The acute
inflammation can be treated with localized ice packs and rest in a sling, but oral anti-inflammatory medications
are also helpful. A cortisone injection directly into the area of the calcium deposit may give relief within a few
hours, when without it the acute severe pain may last for several days.
Do calcium deposits need removal?
If a patient has two or three recurrent episodes of painful symptoms in the shoulder, or if the calcium deposit
appears on x-ray to be enlarging, then it may be appropriate to consider arthroscopic surgery to remove it.
What is involved in arthroscopic surgery to remove calcium?
The surgery is done in the outpatient department under a general anesthesia. There is no pain at all during
the operation and afterwards a mild aching sensation is usually present for a few days until the skin puncture
sites heal. If the calcium erodes a hole in the rotator cuff, then decompression is necessary (removing a
portion of the overhanging bone arthroscopically) and this will cause a little more discomfort for a few days.
Will calcification return once it is removed?
We have never seen a calcification return in the same shoulder once it has been removed.
Can there be any permanent damage caused by calcification?
Yes. A long-term calcification may cause pressure on the rotator cuff tendon which can damage portions of
the tendon permanently.
AC Joint
What is the AC Joint in the shoulder?
The top of the wing bone or scapula is the acromion. The joint formed where the acromion connects to the
collarbone or clavicle is the AC joint. Usually there is a protuberance or bump in this area, which can be quite
large in some people normally. This joint, like most joints in the body, has a cartilage disk or meniscus inside
and the ends of the bones are covered with cartilage. A capsule holds the joint together, and the clavicle is
held in the proper position by two heavy ligaments called coracoclavicular ligaments.
How is the AC Joint usually injured?
The AC joint is injured most often when one falls directly on the point of the shoulder. The trauma will
separate the acromion away from the clavicle, causing a sprain or a true AC joint dislocation. In a mild
injury, the ligaments that support the AC joint are simply stretched (Grade I), but with more severe injury, the
ligaments can partially tear (Grade II) or completely tear (Grade III). In the most severe injury, the end of the
clavicle protrudes beneath the skin and is visible as a prominent bump.
How is an AC Joint separation diagnosed?
Most often the clinical exam will demonstrate tenderness or bruising around the top of the shoulder near the
AC joint, and the suspected diagnosis can be confirmed using an x-ray, which compares the injured side with
the patient's other joint.
What is the proper treatment for a sprained AC Joint?
When a joint is first sprained, conservative treatment is certainly the best. Applying ice directly to the point
of the shoulder is helpful to inhibit swelling and relieve pain. The arm can be supported with a sling that also
relieves some of the weight from the shoulder. Gentle motion of the arm can be allowed to prevent stiffness,
and exercise putty is very helpful to improve function of the elbow, wrist, and hand, but any attempts at
vigorous shoulder mobilization early on will probably lead to more swelling and pain.
How long does it take for a shoulder separation to heal?
Depending on the severity of the injury, it may heal adequately in two to three weeks. In severe cases, the
shoulder may not heal without surgery.
When and why is surgery necessary for AC Joint separations?
Usually surgery is reserved for those cases where there is residual pain or unacceptable deformity in the joint
after several months of conservative treatment. The pain can occur with direct pressure on the joint, such as
with straps from underwear or work clothing. Sometimes there will be catching, clicking, or pain with overhead
activities, such as lifting, throwing, or reaching. Finally, in some people with very thin skin and very little
muscular and soft tissue padding above their shoulders, the prominent clavicle after the separation may be
considered unattractive, since the shoulder can appear to be unbalanced.
Are there other causes of AC Joint pain and disability?
Arthritis can occur as an isolated event in the AC joint, causing stiffness, aching, and sometimes swelling.
Another condition called DCO, or distal clavicle osteolysis, gives a similar picture, usually in young people
who lift heavy weights. This is called "Weightlifter's Shoulder."
What type of surgery can repair AC Joint problems?
The simplest type of surgery for AC joint injury involves resection or removal of the end of the clavicle using
arthroscopic (mini-surgical) techniques (called a Mumford procedure). If the joint becomes painful because
of DCO (weightlifter's shoulder) or arthritis, or the separation is only minor, this technique can be very
satisfactory. When the joint is severely displaced, then a more complex procedure is needed to restore the
position of the clavicle. Usually this operation, called a Weaver-Dunn procedure, is done using a two-inch
incision over the joint. The end of the clavicle is removed, and ligament is transferred from the underside of
the acromion into the cut end of the clavicle to replace the ligaments torn during the dislocation. Soon an
arthroscopic procedure should be available to restore the position of the joint, but at this point, only open
surgery techniques are available.
What is the postoperative treatment and rehabilitation?
Postoperatively, treatment depends on the type of surgery performed. Usually, when the Mumford procedure
is performed using arthroscopic techniques, the arm can be treated with a sling. Bathing is allowed in three
days' time, and elbow, wrist, and hand exercises are begun immediately. Lifting is limited for three weeks, but
following that, progressive exercise and motion activities proceed as the symptoms allow. When a Weaver-
Dunn procedure (rebuilding of the torn ligaments) is needed, approximately two or three weeks is added to
the immobilization time before motion exercises are begun. This time allows the ligament to heal. Otherwise,
the exercise program is the same as that for the Mumford procedure above.
Biceps Tendon
What is the biceps tendon?
The biceps tendon is a long cord-like structure that is located in the front of the shoulder. It originates from
the top of the shoulder socket (the glenoid) and exits the joint through a bony trough (the biceps groove).
Below the shoulder, this tendon becomes the long head of the biceps muscle. The short head of the biceps
is a continuation of the conjoined tendon that originates from a bony hook (the coracoid) at the front of the
shoulder blade. Thus the biceps muscle, which functions to bend the elbow and rotate the forearm, has two
anchor points in the shoulder region.
Who get biceps tendon injuries?
In general, these injuries occur more frequently as we become older. As we age, our tendons lose their
elasticity and slowly become stiffer and more "brittle." The blood supply which nourishes the tendon also
diminishes with age. The "degenerative" processes may be more pronounced in sedentary individuals, but
may be lessened with proper and regular exercise. The well-conditioned individual, however, is not immune
from biceps tendon injuries as over-training can also harm an otherwise healthy tendon.
How do biceps tendon injuries occur?
As mentioned above, age, inactivity, or over-activity can weaken a tendon, which may lead to injury due to
the decreased ability to endure repetitive motions and sudden loads because of its location, from a direct
blow to the front of the shoulder. Some individuals develop bone spurs in their biceps grooves or under the
top of their shoulder blades (the acromion), which can lead to wear and tear of their tendons. A less frequent
injury is a dislocation of the biceps tendon from its groove. This is usually seen in combination with a tear of
the subscapularis tendon or the rotator cuff tendon, which normally help hold the biceps tendon in it groove.
The biceps tendon can also be injured at its attachment site on top of the glenoid. This usually involves an
avulsion, where the tendon is pulled off the bone and rendered unstable.
What happens to the tendon when it is injured?
If the tendon or its sheath (which encases the tendon) is irritated, it becomes inflamed, resulting in pain and
swelling. This condition is called "tendinitis." Mild injuries can also result in microscopic tearing of individual
tendon fibers. As the severity of an injury increases, larger tears can occur to the point where the tendon is
partially torn or even completely ruptured. If a rupture occurs, the long head will usually fall distally toward the
elbow. Biceps muscle function usually remains nearly normal because of its dual attachment proximally.
How are biceps tendon injuries treated?
Initially, rest, ice, and gentle anti-inflammatory medications are all that is usually needed. Sometimes an
injection with a strong anti-inflammatory medication such as cortisone is needed to control the pain and
swelling. Severe cases that fail to improve may require surgical treatment.
What does surgery involve?
Surgical treatment depends on the nature and extent of damage to the tendon. If only a small portion of
the tendon is damaged, a simple arthroscopic shaving (debridement) of the torn fibers may be all that is
needed. If a significant portion is involved, a biceps tenodesis may need to be performed. This is done by
arthroscopically removing the torn tendon stump from inside the shoulder joint and then, through a small
skin incision, attaching the remaining tendon to the bone in the upper arm (humerus). If the biceps tendon
is completely rupture, causing the muscle to bulge in the upper arm, a tenodesis can be done only if the
distal portion remains near the top of the shoulder. A tenodesis is not done if the tendon slides too far distally
because doing so would require unacceptably large incisions. If the tendon has been partially avulsed from
its origin on the top of the glenoid (SLAP lesion), it can be arthroscopically reattached using miniature screws
and sutures.
What is the usual course after surgery?
A simple sling is all that is needed for the first few weeks after surgery. Immediate use of the hand is
encouraged, but only for very light objects. Four to six weeks of healing is required before a gradual return
to moderate or heavy lifting. Desk work and light-duty can usually be resumed within the first week or two.
Return to heavy labor usually takes 2 to 4 months.
Shoulder Arthritis
What is shoulder arthritis?
Arthritis is a condition that occurs in various joints in the body, especially in the knees, hips, and spine. It
can affect any joint, but the shoulder is affected infrequently. When arthritis occurs, the cartilage that covers
the ends of the bones making up the joint breaks down and often flakes off into the joint. The joint becomes
swollen and stiff, and the lining tissue of the joint (the synovium) becomes overgrown. Frequently, spurs will
develop around the margins of the joint and can, sometimes, break off inside. The pain can vary from mild to
very severe, depending upon many factors, including the severity of the disease, the type of arthritis (most are
wear and tear, or degenerative arthritis, but some are caused by rheumatoid disease) and the activity level.
Who usually gets arthritis?
Anyone can develop arthritis, but it most often occurs in middle-aged patients and senior citizens. The
condition may occur spontaneously or as a late result of previous trauma, such as fracture or dislocation. It
also may occur as a result of an inflammatory disease such as rheumatoid arthritis.
How do I know if I have arthritis?
The shoulder joint becomes stiff, feels heavy, and fatigues easily when arthritis is present. The stiffness is
usually worse in the morning, and can slowly improve with "warm up activities." Also, grinding and catching in
the shoulder is a common sign of arthritis.
What tests can the doctor do to prove if arthritis is present?
Most advanced cases of arthritis can be diagnosed with an x-ray evaluation of the shoulder. Sometimes, with
rheumatoid or other types of "inflammatory" arthritis, special blood tests or other evaluations are needed.
What is the best treatment for arthritis of the shoulder?
The treatment of shoulder arthritis depends on how disabling and painful the disease is. Often your doctor
will refer you to a rheumatologist who specializes in treating arthritis with medications. Physical therapy,
particularly hydrotherapy (swimming pool), is very soothing, and helps maintain or regain range of motion
of the joint, and strengthen the surrounding muscles. If the arthritis is advanced, causing severe pain and
disability, then your doctor may consider an operative procedure. Some early arthritis can be treated with
arthroscopic (microsurgical) techniques. With this operation, the doctor will trim out the inflamed synovial
lining tissue and remove debris and pieces of degenerated cartilage. Of course, this will not cure the arthritis,
but frequently can relieve many of the symptoms, at least for a while. In severe disease, the only surgical
treatment is joint replacement. This is a very good operation for pain relief and often will restore some motion,
but it has its limitations. The joint surfaces are surgically replaced through a five-inch incision in the front of
the shoulder, and a metal ball and plastic socket are inserted.
If total shoulder joint replacement is needed, what are some of the risks?
The risks of total shoulder replacement are those of any standard surgical procedure and include infection,
anesthesia risks (including death), nerve and vascular injury about the shoulder, and failure of the operation.
If the operation fails, it may result in stiffness or sometimes a loose joint. If the joint becomes loose, it may
either have to be redone at a future date, or reoperated to have the ligaments or muscles tightened. In the
shoulder joint, this is quite a rare occurrence, although long-term follow-up of more than 10 years is not yet
available.
What is the postoperative treatment after shoulder replacement?
If the shoulder was extremely tight, the doctor prefers to support the arm in a brace after surgery that allows
the muscles and ligaments to heal in a lengthened position. If the shoulder was not particularly tight, then the
arm can be kept in a sling at the side. Exercises begin on the day after surgery, and include movement of the
elbow, wrist and hand, and exercising the grip with putty. Shortly thereafter, rotational pendulum exercises
can be added. Strengthening exercises begin at about three weeks when the brace or sling is removed. This
delay is necessary to allow the tissues that were opened at the time of surgery to heal.
How long will it take my shoulder to improve to its maximum?
The shoulder will generally continue to improve quite steadily up to five to six months after surgery. After that
point, further improvement is very slow; although it has been shown that even after a year or more, activity
can increase as muscle strength continues to improve. It is very important to continue an exercise program to
regain and maintain excellent muscle strength around the new shoulder joint.
Shoulder Exercises
The most common cause of shoulder pain is impingement syndrome. Often called bursitis, cuffitis, or
"thrower's shoulder", it is common to all overhead activities, such as tennis, racquetball, baseball, and
swimming.
It is caused by excessive rubbing of the rotator cuff muscles on the undersurface of the shoulder bone during
overhead activities. This rubbing causes inflammation (swelling and redness), which results in pain about the
shoulder whenever the arm is placed in an overhead position.
One of the causes of impingement syndrome is muscle strength imbalance between the forward throwing
muscles and the "recovery" muscles, which take the arm into an overhead position. These "recovery"
muscles are also known as the Rotator Cuff muscles and are often weaker in strength than the forward
throwing muscles.
Exercises to strengthen the rotator cuff muscles will help, over the long term, to prevent impingement
syndrome and, therefore, shoulder pain.
 Begin by bending forward at the waist, supporting yourself with the
uninvolved arm. Take a light weight (1-2 pounds) and do 15 lifts directly to
the side with the elbow straight. Repeat this exercise set 4 times.
Repeat these sets of exercises (4 sets of 15 lifts) with the arm positioned
45 degrees behind your original position and again at 45 degrees in front
of your original position.
Begin by bending forward at the waist, supporting yourself with the
uninvolved arm. Take a light weight (1-2 pounds) and do 15 lifts directly to
the side with the elbow straight. Repeat this exercise set 4 times.
Repeat these sets of exercises (4 sets of 15 lifts) with the arm positioned
45 degrees behind your original position and again at 45 degrees in front
of your original position.
You should use enough weight so that these exercises feel difficult. You
should add weight as your muscles increase in strength.
As you do these exercises, you should feel the muscles around the shoulder blade getting a workout. These
shoulder blade muscles are the rotator cuff muscles.
Remember that these exercises are meant to be helpful over the long term and will not produce an
immediate cure. If you are active in overhead sports, you should be doing these exercises on a regular basis.
rehabilitation After Shoulder Surgery
 Rehabilitation of the shoulder should begin the first several days after surgery. Phase I includes Passive
Range of Motion of your shoulder, and lasts for the first 3-4 weeks after surgery. During this time, movement
of the shoulder should be done by a partner (friend, parent, spouse, physical therapist, or athletic trainer).
This avoids stiffness of the shoulder while protecting the shoulder muscles.
Rehabilitation of the shoulder should begin the first several days after surgery. Phase I includes Passive
Range of Motion of your shoulder, and lasts for the first 3-4 weeks after surgery. During this time, movement
of the shoulder should be done by a partner (friend, parent, spouse, physical therapist, or athletic trainer).
This avoids stiffness of the shoulder while protecting the shoulder muscles.
1. With your shoulders square to your assistant, he/she lifts the elbow forward as far as can be tolerated and
holds this position for a count of 10.
2. With your assistant to your side, he/she lifts the elbow to the side as far as can be tolerated and holds this
position for a count of 10.
3. With your assistant facing you, and the involved elbow held at the side, the hand and wrist are moved
outwards as far as can be tolerated and held for a count of 10.
4. Finally, with the arm either in or out of the sling, lean forward and let your shoulder and arm dangle. Make
small circles with your elbow and/or fingers. Make progressively bigger and bigger circles. Perform these
exercises 2-3 times per day. After the first month, Phase II will include further physical therapy to work on more
range of motion and strengthening of your shoulder.
|
For Our Patients
Existing patients may utilize these convenient links to access forms, educational materials and manage their accounts.
Medical Questionnaire
Patient Forms
Convenient, Online
Patient Forms Are
Coming Soon!
Pay My Bill
INSURANCE PROVIDERS WE PARTICIPATE WITH:
Commercial
Blue Cross/Blue Shield
DMBA
HMA
HMAA
HMSA PPO & HMSA HMO
MDX
UHA
Government
Medicare
Medicaid
OHANA/Wellcare
Triwest/Tricare
UHC- Medicare Advantage
Other
Workers Compensation
No-Fault
|

 In the past, treatment of orthopedic injuries involved extensive surgery,
including large incisions, a hospital stay and a prolonged recovery period.
But arthroscopy has revolutionized the treatment of joint injuries.
In the past, treatment of orthopedic injuries involved extensive surgery,
including large incisions, a hospital stay and a prolonged recovery period.
But arthroscopy has revolutionized the treatment of joint injuries. diameter), but appear much larger when viewed through an arthroscope. This is a probe
used for examination of internal structures.
diameter), but appear much larger when viewed through an arthroscope. This is a probe
used for examination of internal structures.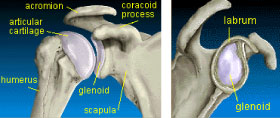 The two main bones of the shoulder are the humerus
and the scapula (shoulder blade). The end of the
scapula, called the glenoid, meets the head of the
humerus to form a glenohumeral cavity that acts as a
flexible ball-and-socket joint.
The two main bones of the shoulder are the humerus
and the scapula (shoulder blade). The end of the
scapula, called the glenoid, meets the head of the
humerus to form a glenohumeral cavity that acts as a
flexible ball-and-socket joint. A ring of fibrous cartilage surrounds the glenoid and stabilizes
the joint. This is called the labrum.
A ring of fibrous cartilage surrounds the glenoid and stabilizes
the joint. This is called the labrum. Rehabilitation of the shoulder should begin the first several days after surgery. Phase I includes Passive
Range of Motion of your shoulder, and lasts for the first 3-4 weeks after surgery. During this time, movement
of the shoulder should be done by a partner (friend, parent, spouse, physical therapist, or athletic trainer).
This avoids stiffness of the shoulder while protecting the shoulder muscles.
Rehabilitation of the shoulder should begin the first several days after surgery. Phase I includes Passive
Range of Motion of your shoulder, and lasts for the first 3-4 weeks after surgery. During this time, movement
of the shoulder should be done by a partner (friend, parent, spouse, physical therapist, or athletic trainer).
This avoids stiffness of the shoulder while protecting the shoulder muscles.