Patient Resources
Your Ankle/Foot
Anatomy of the Ankle
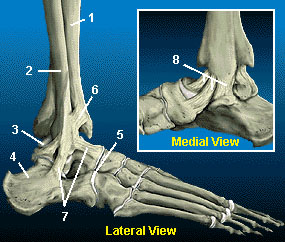
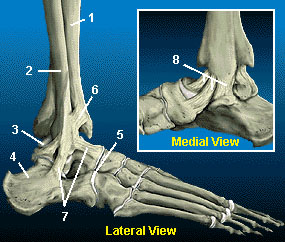 The true ankle joint is composed of three bones, seen
here from a front (or anterior) view: the tibia (1) which
forms the inside, or medial, portion of the ankle; the
fibula (2) which forms the lateral, or outside portion
of the ankle; and the talus (3) underneath. The true
ankle joint is responsible for up and down motion of
the foot.
The true ankle joint is composed of three bones, seen
here from a front (or anterior) view: the tibia (1) which
forms the inside, or medial, portion of the ankle; the
fibula (2) which forms the lateral, or outside portion
of the ankle; and the talus (3) underneath. The true
ankle joint is responsible for up and down motion of
the foot.
Beneath the true ankle joint is the second part of the
ankle, the subtalar joint, which consists of the talus (3)
on top and calcaneus (4) on the bottom. The subtalar
joint allows side-to-side motion of the foot.
The ends of the bones in these joints are covered
by articular cartilage (5). The major ligaments of the
ankle are: the anterior tibiofibular ligament (6), which
connects the tibia to the fibula; the lateral collateral
 ligaments (7), which attach the
fibula to the calcaneus and gives the ankle lateral stability; and, on the medial side of the
ankle, the deltoid ligaments (8), which connect the tibia to the talus and calcaneus and
provide medial stability.
ligaments (7), which attach the
fibula to the calcaneus and gives the ankle lateral stability; and, on the medial side of the
ankle, the deltoid ligaments (8), which connect the tibia to the talus and calcaneus and
provide medial stability.
These components of your ankle, along with the muscles and tendons of your lower leg,
work together to handle the stress your ankle receives as you walk, run and jump.
Plantar Fasciitis
Plantar fasciitis (inflammation of the plantar fascia) is the most common cause of heel
pain seen by an orthopedist. It is common in several sub-groups of people, including
runners and other athletes, people who have jobs that require a fair amount of walking or standing (especially
if it is done on a hard surface), and in some cases it is seen in people who have put on weight — either by
dietary indiscretion or pregnancy.
The plantar fascia is a broad ligament-like structure that extends from the heel bone to the base of the toes,
acting like a thick rubberband on the bottom arch of the foot. With a few extra pounds on board, or with
activities such as exercise, the plantar fascia can develop microtrauma at its insertion into the heel bone, or
anywhere along its length. This causes pain, which can be quite severe at times.
One disturbing fact about plantar fasciitis is that it sometimes takes many months to resolve. Indeed, it takes
approximately 6 months for 75% of people to recover from this problem. 98% of people seem to be better at
12 months.
Treatment consists of 3 stages
Stage 1 involves prescribing the patient a heel cushion to decrease shock absorption of the plantar fascia, as
well as a short course of medication to decrease inflammation in the heel.
Stage 2 may involve cortisone injections into the heel region, if Stage 1 has failed to bring significant relief.
Other modalities in Stage 2 include orthotics, taping, physical therapy and night splinting.
Stage 3 is for those who have had plantar fasciitis for one year or longer or whose symptoms are severe and
preventing them from their job or recreation. It involves a surgical release of part of the insertion of the plantar
fascia. However, this surgery is rare, as most people do have significant relief from non-surgical treatment.
Club Foot
 Clubfoot Birth deformities of the foot fall into two categories: 1) positional deformities
— "packaging defects" of the foot, and 2) malformations — "manufacturing defects" in
which the parts are incorrectly formed. A true clubfoot is a malformation. The bones,
joints, muscles, and blood vessels of the limb are abnormal. The medical term for this is
"talipes equinovarus" — relating the shape of the foot to a horses hoof. Don't ask why!
Clubfoot Birth deformities of the foot fall into two categories: 1) positional deformities
— "packaging defects" of the foot, and 2) malformations — "manufacturing defects" in
which the parts are incorrectly formed. A true clubfoot is a malformation. The bones,
joints, muscles, and blood vessels of the limb are abnormal. The medical term for this is
"talipes equinovarus" — relating the shape of the foot to a horses hoof. Don't ask why!
Clubfoot can be recognized in the infant by examination. The foot is in-turned, stiff and
cannot be brought to a normal position. Children with the condition should be referred to
an orthopedic surgeon for complete evaluation and treatment of the deformity.
This photo of a clubfoot shows the foot is inwardly rotated (towards the big toe) and supinated (turned on its
side towards the other foot). In walking position, this child would walk on the outside border of the foot.
 This rear view of the foot shows the heel retracted towards the leg (equinus).
Note the medial (inner) crease and curved lateral (outer) border of the foot.
This foot cannot be brought to plantigrade position, meaning flat on the floor.
The usual treatment of clubfoot is a series of corrective casts applied early
in life to stretch the foot into as corrected a position as possible. Frequently
surgery is also needed to release the stiff and misaligned joints of the foot to
make it "plantigrade" or flat to the floor.
This rear view of the foot shows the heel retracted towards the leg (equinus).
Note the medial (inner) crease and curved lateral (outer) border of the foot.
This foot cannot be brought to plantigrade position, meaning flat on the floor.
The usual treatment of clubfoot is a series of corrective casts applied early
in life to stretch the foot into as corrected a position as possible. Frequently
surgery is also needed to release the stiff and misaligned joints of the foot to
make it "plantigrade" or flat to the floor.
The result of such treatment is usually good with a adequate foot for normal footwear, sports, and cosmesis.
Sometimes later in life or late childhood, there can be pain in the foot necessitating special shoe modifications
such as arch supports, or even additional corrective surgery.
A true clubfoot is usually stiff and will lack normal motion, be smaller than a normal foot, and the muscularity
of the calf will be noticeably smaller. Sports, exercise, and corrective surgery can be used to strengthen
and realign the foot, but there is always a distinct difference between the normal side and the clubfoot.
The treatment of clubfoot is rather involved, and best managed by orthopedic surgeons experienced in the
techniques mentioned above.
Sever's Disease
Sever's disease is a painful condition of the heel in growing children. It may frequently occur after significant
activities such as running or jumping. The children have difficulty putting pressure on the heel and frequently
will begin walking on their toes.
The actual pathology of the condition is one of more of an overuse syndrome in which the growth plate of
the heel may become slightly displaced, causing pain. Biopsies of similar conditions have shown changes
consistent with separation of the cartilage. The condition is very similar to Osgood-Schlatter's disease, which
occurs at the knee.
The general feeling is that there is stress placed on the growth plate and this causes microfractures between
the growth plate and the rest of the bone of the heel. The condition is self-limited, however, it may take a
prolonged period of time until it completely resolves.
Treatment revolves around decreasing activity. Our usual treatment has been putting children in a boot in
slight equinus, or a cast with the foot in slight equinus, thereby decreasing the tension on the heel cord,
which in turn pulls on the growth plate at the heel. As the pain resolves, children are allowed to go back to full
activities.
Complete resolution may be delayed until growth of the foot is complete — when the growth plate fuses to the
rest of the bone of the heel.
|
For Our Patients
Existing patients may utilize these convenient links to access forms, educational materials and manage their accounts.
Medical Questionnaire
Patient Forms
Convenient, Online
Patient Forms Are
Coming Soon!
Pay My Bill
INSURANCE PROVIDERS WE PARTICIPATE WITH:
Commercial
Blue Cross/Blue Shield
DMBA
HMA
HMAA
HMSA PPO & HMSA HMO
MDX
UHA
Government
Medicare
Medicaid
OHANA/Wellcare
Triwest/Tricare
UHC- Medicare Advantage
Other
Workers Compensation
No-Fault
|

 The true ankle joint is composed of three bones, seen
here from a front (or anterior) view: the tibia (1) which
forms the inside, or medial, portion of the ankle; the
fibula (2) which forms the lateral, or outside portion
of the ankle; and the talus (3) underneath. The true
ankle joint is responsible for up and down motion of
the foot.
The true ankle joint is composed of three bones, seen
here from a front (or anterior) view: the tibia (1) which
forms the inside, or medial, portion of the ankle; the
fibula (2) which forms the lateral, or outside portion
of the ankle; and the talus (3) underneath. The true
ankle joint is responsible for up and down motion of
the foot. ligaments (7), which attach the
fibula to the calcaneus and gives the ankle lateral stability; and, on the medial side of the
ankle, the deltoid ligaments (8), which connect the tibia to the talus and calcaneus and
provide medial stability.
ligaments (7), which attach the
fibula to the calcaneus and gives the ankle lateral stability; and, on the medial side of the
ankle, the deltoid ligaments (8), which connect the tibia to the talus and calcaneus and
provide medial stability. Clubfoot Birth deformities of the foot fall into two categories: 1) positional deformities
— "packaging defects" of the foot, and 2) malformations — "manufacturing defects" in
which the parts are incorrectly formed. A true clubfoot is a malformation. The bones,
joints, muscles, and blood vessels of the limb are abnormal. The medical term for this is
"talipes equinovarus" — relating the shape of the foot to a horses hoof. Don't ask why!
Clubfoot Birth deformities of the foot fall into two categories: 1) positional deformities
— "packaging defects" of the foot, and 2) malformations — "manufacturing defects" in
which the parts are incorrectly formed. A true clubfoot is a malformation. The bones,
joints, muscles, and blood vessels of the limb are abnormal. The medical term for this is
"talipes equinovarus" — relating the shape of the foot to a horses hoof. Don't ask why! This rear view of the foot shows the heel retracted towards the leg (equinus).
Note the medial (inner) crease and curved lateral (outer) border of the foot.
This foot cannot be brought to plantigrade position, meaning flat on the floor.
The usual treatment of clubfoot is a series of corrective casts applied early
in life to stretch the foot into as corrected a position as possible. Frequently
surgery is also needed to release the stiff and misaligned joints of the foot to
make it "plantigrade" or flat to the floor.
This rear view of the foot shows the heel retracted towards the leg (equinus).
Note the medial (inner) crease and curved lateral (outer) border of the foot.
This foot cannot be brought to plantigrade position, meaning flat on the floor.
The usual treatment of clubfoot is a series of corrective casts applied early
in life to stretch the foot into as corrected a position as possible. Frequently
surgery is also needed to release the stiff and misaligned joints of the foot to
make it "plantigrade" or flat to the floor.